Case Management
CenCal Health’s case management (CM) services are provided by registered nurses, social workers, and transitional care coordinators via telephone. Case Management (CM) services are offered to both adult and pediatric members.
Our Case Management Services help members who:
- have complex medical or behavioral health conditions
- have high psychosocial risk factors
- need assistance navigating through the health care system and continuum of care
Upon referral, a Case Manager will screen for appropriateness and triage for the urgency of initiating CM services. If the member accepts Case Management, the Case Manager will formulate a Plan of Care and inform the member’s PCP. If the member declines Case Management, the Case Manager will notify the referral source.
Submitting a Case Management Referral is easy.
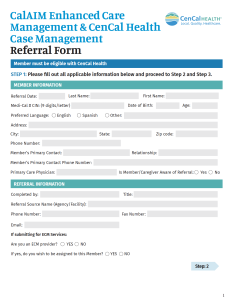 Download the CalAIM Enhanced Care Management & CenCal Health Case Management Referral Form and fax the completed form to CenCal Health’s Case Management Department at (805) 681-8260.
Download the CalAIM Enhanced Care Management & CenCal Health Case Management Referral Form and fax the completed form to CenCal Health’s Case Management Department at (805) 681-8260.
Include any additional clinical information that may help the case manager address the needs of the member.
Examples of Cases that Should Be Referred to Case Management Services:
Frequent hospital admissions or readmissions (e.g., four hospital visits in one year) within 30 days of discharge.
Frequent Emergency Department use.
Members who need education on their chronic medical condition and /or medication adherence.
Unstable medical conditions warranting closer monitoring (e.g. CHF, uncontrolled diabetes, exacerbating asthma or COPD).
Assistance with coordination to community resources (e.g. Food Bank, Meals on Wheels, Family Resource Centers, and/or Unity Shop).
Coordination of care is needed for members to receive medically necessary services within or outside the Health Plan’s provider network (local Education Agency, Regional centers, CCS).
Complex or chronic medical condition, including those affecting multiple organ systems or complicated therapy (e.g. transplants, cancer, ESRD, terminal illness without hospice services).
Members with fragile conditions, including cognitive changes needing assistance with care coordination or care transitions.


