


Pharmacy Services
CenCal Health is committed to providing consistent, compassionate, and local support to all CenCal Health providers and members.
CenCal Health’s Pharmacy Team is comprised of Pharmacist and Pharmacy Technician staff. Our Pharmacy Team is ready to assist our provider network and membership with pharmacy-related inquires and education.
Medi-Cal Rx: Medi-Cal Pharmacy Benefit
Effective January 1, 2022, CenCal Health’s Pharmacy benefit called Medi-Cal Rx is administered through DHCS and its vendor, Magellan Medicaid Administration. Magellan provides a comprehensive suite of administrative services as directed by DHCS, which includes claims management/adjudication, prior authorization, utilization management, and customer/support.
Medi-Cal Rx is responsible for administering the following when billed by a pharmacy on a pharmacy claim:
- Covered Outpatient Drugs, including Physician-Administered -Drugs (PADs)
- Medical Supplies
- Enteral Nutritional Products
Additional information regarding Medi-Cal Rx can be found in the “Medi-Cal Rx News” tab below and directly from the DHCS Medi-Cal Rx web site.
For additional assistance contact Medi-Cal Rx Customer Service at: (800) 977-2273
You may also want to visit the Medi-Cal Rx Communication page for any upcoming bulletins and news.
CenCal Health Pharmacy Services: Medical Pharmacy Management
CenCal Health and the Pharmacy Services Team will be responsible for a variety of activities including, but not limited to: oversight of clinical pharmacy adherence, Drug Utilization Review (DUR) and all utilization management associated with pharmacy services (Physician-Administered-Drug) billed on a medical and institutional claim. CenCal Health defines the utilization management of Physician-Administered-Drugs on the medical benefit as Medical Pharmacy Management.
Additional information and education resources for CenCal Health’s Medical Pharmacy Management Program can be found on our Medical Pharmacy Management page.
Medi-Cal Rx: COVID-19 Vaccine Update
The new commercial COVID-19 vaccines for the OmicronXBB1.5 variant are now a covered Medi-Cal Rx benefit. Reimbursement for the vaccine will include the cost of the commercial vaccines (in addition to the $40 incentive fee).
For members 6 months through 2 years of age, coverage of the vaccine will be available only through the Vaccines For Children (VFC)program. Products remain federally funded. To locate an eligible provider, visit https://eziz.org/ or call1-877-243-8832. Claims submitted to Medi-Cal Rx for members younger than 3 years of age will reject with Reject Code 60 – Product/Service Not Covered for Patient Age. For more information regarding this age restriction update refer to the Medi-Cal Rx Update Commercial COVID-19 Vaccine Coverage for Children . COVID-19 vaccines are a Medi-Cal Rx pharmacy benefit for members 3 years of age and older.
Uninsured and underinsured adults may obtain freeCOVID-19 vaccines through the Centers for Disease Control and Prevention’s (CDC) Bridge Access Program. The vaccines can be accessed through local pharmacies and health care providers, including ederally Qualified Health Centers (FQHCs). For additional details, see the guidance from California Department of Public Health (CDPH)’s California Bridge Access Program.
Even with the recent commercialization, DHCS will continue to carve out the COVID-19 vaccines and associated administration fees from the Medi-Cal managed care delivery system and will reimburse providers under Medi-Cal fee-for-service for medical, pharmacy, and outpatient claims. This will continue until further notice, at least until December 31, 2024. MCPs will be notified if this changes.
COVID-19 Antigen Over-the-Counter Test Coverage Updates, Effective November 1, 2023
Self-administered COVID-19 antigen test kits will remain a Medi-Cal Rx covered pharmacy benefit, subject to utilization and board of pharmacy prescription billing requirements.
The following criteria applies for coverage of these tests as a Medi-Cal Rx pharmacy benefit:
- Restricted for the diagnostic condition of suspected COVID-19
- Restricted to up to 8 tests total (4 kits with 2tests per kit).
- No refills allowed. The member would need to obtain a new prescription for each dispensing
- Dispensed from a Medi-Cal Rx pharmacy provider, written on a prescription signed by a licensed prescriber or a pharmacist
New November1, 2023
- Pharmacy providers are required to have one-on-one documented contact (in person, telehealth, or phone) with the member or caregiver prior to dispensing COVID-19 EUA (Emergency Use of Authorization)tests
- The member/caregiver must request the pharmacy provider dispense COVID-19 OTC EUA tests
For more information regarding the COVID-19 Antigen Test Kits click here.
Medi-Cal Rx Reinstatement Plan
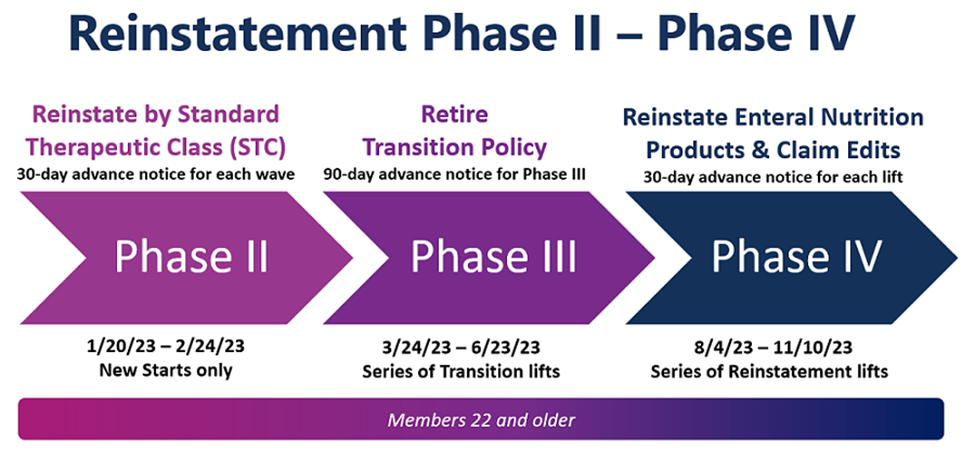
Key Reinstatement Dates
- January 20, 2023: Phase II, Wave 1 begins for new starts only.
- February 24, 2023: Phase II, Wave 2 begins.
- March 24, 2023-June 23, 2023: Series of Transition Lifts
- August 4, 2023: Phase IV, Lift 1 was implemented.
- September 22, 2023: Phase IV, Lift 2 was implemented.
- October 13, 2023: Phase IV, Lift 3 was implemented.
- November 10, 2023: Phase IV, Lift 4 will be implemented, End of Transition Policy
Reinstatement Spotlight: Weekly publication released every Friday by Medi-Cal Rx to provide essential information.
Medi-Cal Rx Spotlight Publications can be viewed by signing up for Medi-Cal Rx Subscription Service or by visiting Medi-Cal Rx Bulletins & News
Medi-Cal Rx Retirement of the Transition Policy Begins March 24, 2023
Medi-Cal Rx will initiate the first of a series of transition policy lifts for beneficiaries 22 years of age and older starting March 24, 2023. A transition lift is the retirement or phasing out of the transition policy for identified Standard Therapeutic Classes (STCs) that lifts the override of a Prior Authorization Requirement. Identified STCs will now require a Prior Authorization for members currently receiving a medication in the STCs impacted by the transition policy retirement. Providers should consider covered therapies that do not require a prior authorization or submit a prior authorization if a change in therapy is not appropriate.
Key Reinstatement Publications
February 13, 2023-Phase III, Lift 1
April 21, 2023-Phase III, Lift 2
May 19,2023-Phase III, Lift 3
June 23,2023-Phase III, Lift 4
Prior Authorization Requirements for Enteral Nutrition Products
July 3, 2023-Phase IV, Lift 1
September 22, 2023-Phase IV, Lift 2
October 13, 2023-Phase IV, Lift 3
30-Day Countdown: Phase IV, Lift III: Reinstatement of Reject Code 76: Plan Limitations Exceeded
November 10, 2023-Phase IV, Lift 4
30-Day Countdown: Phase IV, Lift 4: End of Transition Policy
Additional information regarding this transition policy and a list of STCs included in this transition can be found on the Medi-Cal Rx Education and Outreach page by selecting Medi-Cal Rx Reinstatement.
For any provider inquiries regarding the Medi-Cal Rx Reimplementation Plan, call the CenCal Health Pharmacy Department at (805)562-1080.
For questions regarding the reinstatement plan, please contact Medi-Cal Rx at (800) 977-2273. The CenCal Health Pharmacy Department can also assist with inquires at (805) 562-1080.
Medi-Cal Rx Resources and Contracted Drug List (CDL)
Now Available: Medi-Cal Rx Enteral Nutrition Prior Authorization Form
Medi-Cal Rx Searchable Drug Lookup & Contracted Drug List
Medi-Cal Rx Contract Drug List
Find a Pharmacy Search Tool
Medi-Cal Rx Support Services
The following document will provide the processing information for Medi-Cal Rx (i.e. BIN, PCN & Group) and additional payer information.
Medi-Cal Rx Support Services and Key Payer Sheet Details
Pharmacies requesting additional operational claims support please contact:
Medi-Cal Rx Customer Service Center at: (800) 977-2273


