CenCal Health Physician Administered (PAD) Drug List.
For a list of PADs that require a TAR or may have a preferred alternative product, please use the CenCalHealth Physician Administered Drug (PAD) List.
Contact Us
(805) 562-1080
Monday – Friday
8 – 5 pm
Medical Pharmacy Management
CenCal Health is committed to providing our member with access to high-quality health care. To ensure our members receive quality care, CenCal Health Pharmacy Services has implemented a Medical Pharmacy Management Program to identify utilization management opportunities for Physician-Administered-Drugs billed on a medical and institutional claim.
Physician Administered Drugs (PADs) through CenCal Health’s Medical Pharmacy Program include all infused, injectable drugs provided or administered to a member that is billed by a provider on a medical claim by a Procedure Code (i.e. J-Code). These providers include, but are not limited to, physician offices, clinics, and hospitals.
Physician-Administered-Drugs(PAD) Authorization Requests
Certain PAD drugs require prior authorization to ensure medical necessity prior to receiving the drug therapy. Any request for a PAD medication via Procedure Code (i.e. J-Code) requiring a prior authorization, administered at a provider’s office or infusion/hospital facility, must be submitted as a treatment authorization request (Treatment Authorization Request- TAR). Guidance on how to submit a TAR can be found on CenCal Health’s Authorization Page.
Completing Treatment Authorization Requests(TARs) will help expedite the claims processing. If you do not obtain approval, your claims may be delayed or denied until we receive the information needed to establish medical necessity.
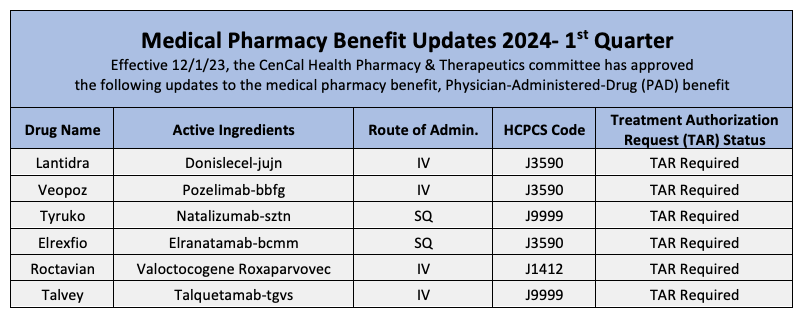
For a list of PADs that require a TAR or may have a preferred alternative product, please use the CenCalHealth Physician Administered Drug (PAD) List. The list is updated quarterly and allows providers to look at specific physician administered drug codes that require prior authorization. Details on the preferred or non-preferred status of certain codes is also displayed in the document. Information on codes not displayed on the CenCal Health Medical Drug List can be found by visiting the CenCal Health Procedures Requiring a TAR tool on the CenCal Health website and Provider Portal.
As a reminder, all pharmacy benefits billed on a pharmacy claim have transitioned to Medi-Cal Rx and are no longer the responsibility of CenCal Health. In addition, there are 5 classes of medications that are carved out of the CenCal Health benefit and are to be reviewed/billed to the State of CA Medi-Cal for authorization consideration and reimbursement for both pharmacy and medical claims.
Medical Pharmacy Management Criteria
Medical Pharmacy Management Criteria
CenCal Health uses written objective criteria based on sound clinical evidence in making utilization decisions based on medical necessity. CenCal Health’s policy on the adoption and development of clinical utilization management criteria defines eligible criteria sources, and the process for development, adoption, and review of clinical criteria. CenCal Health ensures that its UM authorization decisions for its members’ care is based on medical necessity of a requested service consistent with members handbook and covered benefits and in accordance with California State Criteria and California Children’s Services (CCS).
Medical Pharmacy Management Criteria is defined as clinical criteria utilized to review authorization requests for authorization of pharmaceuticals (i.e. Physician Administered Drugs) requested on CenCal Health’s medical benefit. The authorizations rendered on the medical benefit are ultimately associated with claim adjudication on a medical, institutional claim on CenCal Health’s Medical Benefit. Medical Pharmacy Management clinical criteria sets are adopted and maintained by a committee comprised of network doctors and pharmacists called the Pharmacy and Therapeutics Committee.
Medical Pharmacy, PAD Approved Criteria sets include:
Magellan Rx Management Library of Medical Necessity Guidelines
Evidence-based clinical guidelines used for decision-making on physician-administered-drugs based on medical literature, nationally recognized guidelines published in all fields of medicine, practice observations, and database analyses. Sources used in development and adoption of guidelines and algorithms are derived from multiple sources: FDA labeling, pivotal clinical trials, CMS-approved compendia (NCCN, Clinical Pharmacology, LexiComp Lexi-Drugs, Micromedex DrugDex, AHFS-DI), evidence-based clinical practice guidelines, published peer-reviewed literature, and input from key opinion leaders.
Department of Health Care Services(DHCS)
- Medi-Cal Provider Bulletins and Manuals
- Medi-Cal Managed Care All Plan Letters
- California Children’s Services (CCS) Program criteria, guidelines, and Numbered Letters when applicable
- Includes information on Medi-Cal and CCS services, programs, and claim reimbursement. Medi-Cal bulletins and manuals are available in its entirety free of charge: click here
When used as the basis of a decision to modify, delay, or deny services in a specific case, UM Criteria/Guidelines are disclosed to the member and provider (inclusive of network practitioners as well as out-of-network practitioners) and the Member in that specific case.
A specific clinical criteria for a PAD is available upon request by a member by contacting CenCal Health Member Services at 1-(877) 814-1861. A provider requesting a specific clinical criteria is available upon request by contacting the CenCal Health Pharmacy Department at (805) 562-1080.
Preferred Physician-Administered-Drug (PAD) Program
Medical Pharmacy Benefit
CenCal Health’s Medical Pharmacy Management program includes preferred PADs on the medical benefit. The CenCal Health Preferred PAD Program promotes the use of cost effective, equally efficacious drugs when medically appropriate. The program is developed and maintained by a committee comprised of doctors and pharmacists called the Pharmacy and Therapeutics Committee. The committee makes decisions based on information about the drug’s safety, effectiveness and associated clinical outcomes.
CenCal Health’s preferred biosimilars are for the following physician administered drugs:
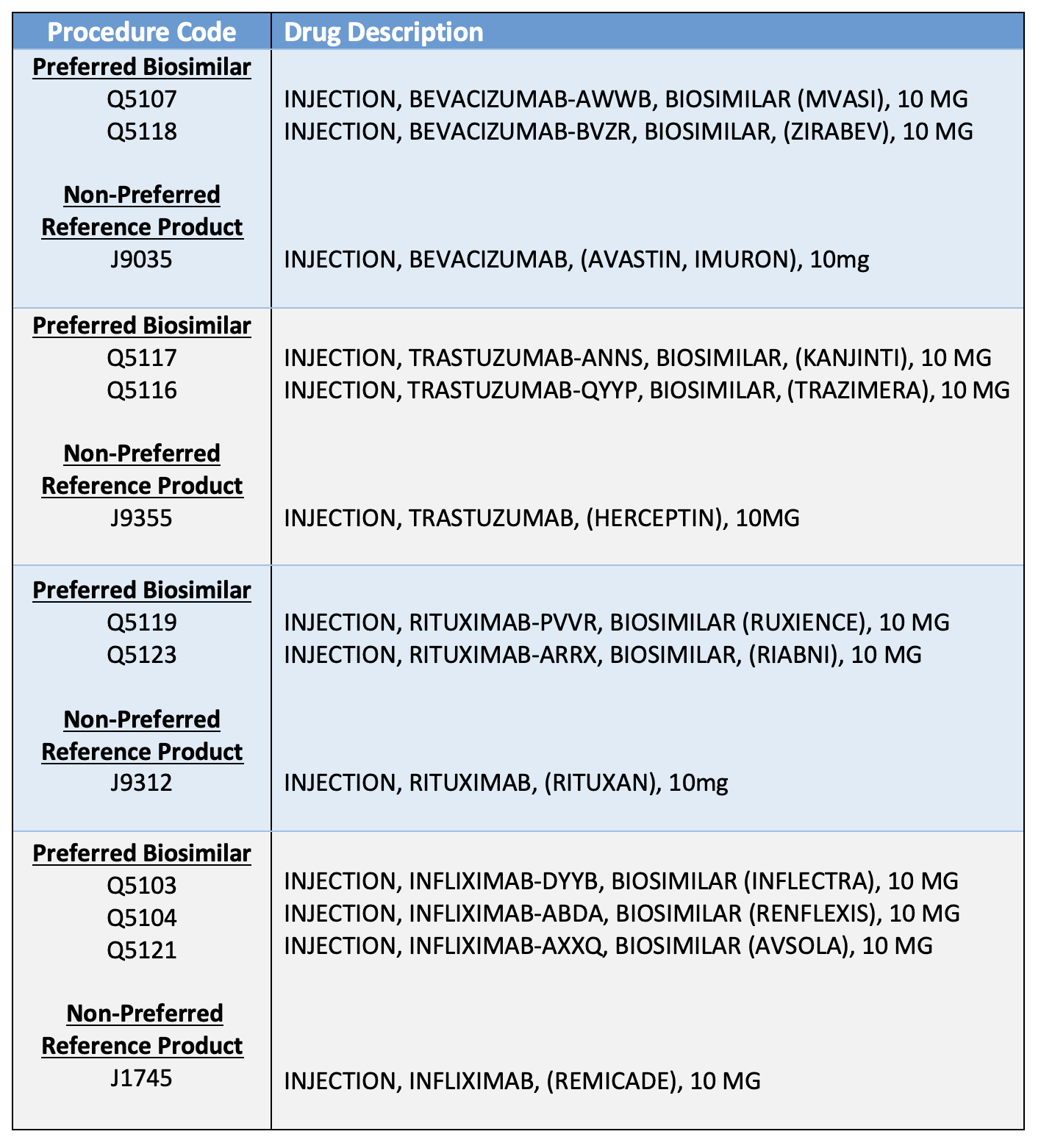
All affected codes remain as TAR required, but at least one of the preferred biosimilar products must be tried and failed before consideration of coverage of the reference product. The biosimilar products are not interchangeable with the reference product and will require new orders. Biosimilar products are highly similar and have no clinically meaningful differences from an existing FDA-approved reference product.
If you have questions or need additional information, please contact CenCal Health Pharmacy Department at(805) 562-1080.